Artificial Intelligence is new frontier in diagnosing endometriosis
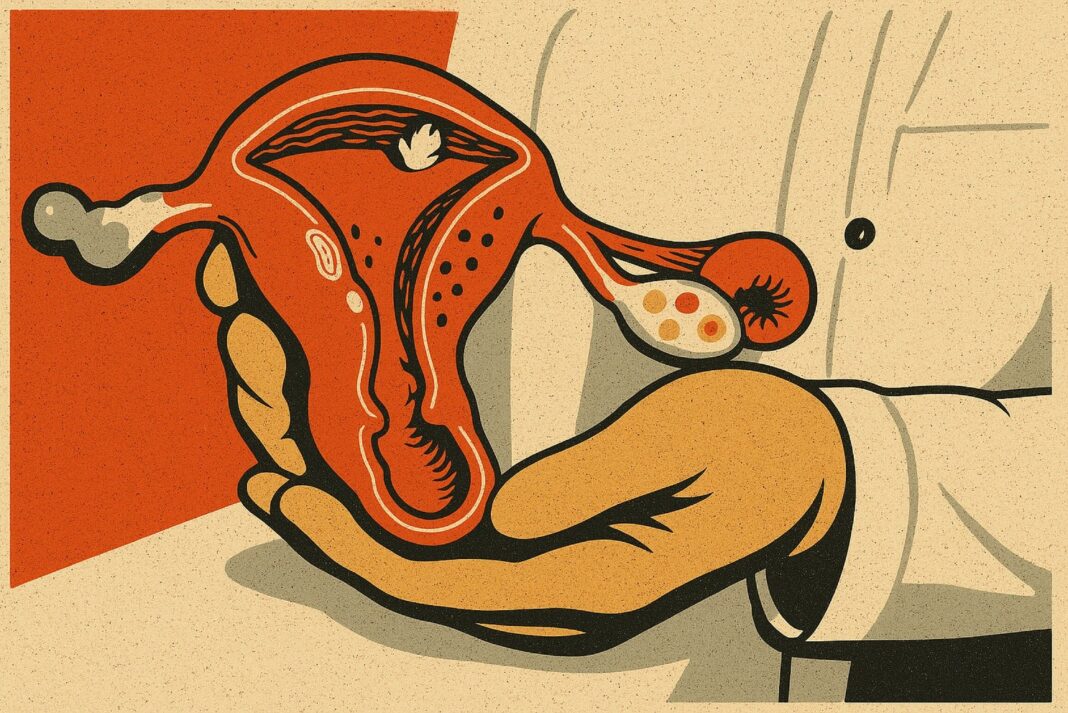
Roughly one in ten women worldwide is affected by endometriosis — a condition as elusive as it is painful. Often described as a “master of disguise”, endometriosis can hide beneath the peritoneal layer, cling to the uterine ligaments, or even mimic healthy tissue. When a lesion is missed, the consequences can be profound: years of chronic pain, infertility, or repeated surgeries.
Even the most experienced surgeons can struggle to identify every sign of the disease. The human eye and traditional laparoscopic tools have limitations. To address these gaps, a European research project called FEMaLe (Finding Endometriosis using Machine Learning) set out to revolutionize how endometriosis is detected and treated in the operating room.
Funded under the European Union’s Horizon 2020 program, FEMaLe received €5,944,134.50 in contributions and ran from 2021 to the end of 2024. The project was coordinated by Aarhus University in Denmark, under the leadership of Ulrik Bak Kirk, chief consultant and project coordinator.
The diagnostic challenge
«We needed to make the invisible visible», explains Kirk. «So, we brought technology to a space that has been neglected for decades.» FEMaLe combined artificial intelligence and computer vision to analyze vast datasets, including clinical records, patient questionnaires, and genetic information. Unlike traditional diagnostics, which often rely on isolated symptoms or imaging, the AI system was trained to detect subtle patterns in large amounts of heterogeneous data. The goal was to identify early indicators of the disease and support more precise, individualized treatment.
At the core of the project is a real-time computer vision algorithm, trained to recognize nine distinct types of endometriotic lesions directly from laparoscopic video footage. The deep learning system analyzes surgical video streams and highlights potential lesions on the surgeon’s screen, offering enhanced visibility and precision during operations.
Importantly, FEMaLe’s system adheres to the principles of Trustworthy AI. The tool is not an autonomous operator but a transparent assistant: surgeons retain full control, and the AI’s predictions are presented as suggestions, not commands. This design was shaped by feedback from clinicians across Europe, collected through interviews and live testing in Denmark, France, and Italy.

Professor Nicolas Bourdel from SurgAR in France (far left), who uses artificial intelligence to diagnose and optimise this deeply complicated surgery. Patient Adrienn Salamon from Hungary (left), who has also helped develop the Lucy app that we use in FEMaLe
Endometriosis Advocate Lone Hummelshøj from England (right), who runs the initiative endometriosis.org
Policy Officer Jerome De Barros from the European Commission(centre).
From data to action
Surgeons described recurring challenges in endometriosis surgery: lesions hidden beneath tissue surfaces, the risk of damaging nearby organs and nerves, scar tissue from previous operations, and the importance of preserving fertility. The growing influence of social media – often spreading misinformation or raising unrealistic expectations – has added further complexity to patient management.
Against this backdrop, many clinicians saw the AI-assisted tool as a valuable support, particularly for less experienced surgeons. Even when a lesion appeared at the edge of the camera view, the system’s alerts could redirect the surgeon’s attention. While the tool may not shorten operation times, it improves safety and diagnostic accuracy, which is a meaningful trade-off.
Translating research into clinical and digital innovation
To bring the technology closer to clinical use, the FEMaLe team integrated the algorithm into an augmented reality (AR) platform developed by the company SURGAR. In this configuration, laparoscopic video is processed in real time, with suspected lesions visually outlined on the display. Testing confirmed that the system maintained its accuracy and responsiveness even after full software integration. These tools not only improve lesion detection but also hold potential for standardizing surgical practices across different healthcare systems. They may help address long-standing gaps in surgical training by accelerating skill acquisition and reducing diagnostic variability.
Throughout its development, FEMaLe implemented a range of coordinated actions. Project management was enhanced through the use of the Half Double Institute’s Methodology, ensuring real-time tracking, reflective learning, and stronger stakeholder engagement. Ethical and inclusive research frameworks guided the project’s direction, with white papers and public outreach efforts such as «Seminar Q: Citizen Science» and the exhibition «Overlooked Body» at the Science Museerne in Aarhus.
The project provided crucial insights into the prevalence of endometriosis, symptom patterns, and diagnostic delays. This epidemiological data helped train machine learning models for early detection. On the genetic front, researchers used polygenic scores from the largest genome-wide association study (GWAS) to date, identifying potential biomarkers like PAEP and LPA for endometrioma. These findings were presented at leading conferences and even informed policy discussions in the Danish Parliament.
The FEMaLe project also supported the development of digital health tools. The Lucy App, with over 20,000 users and 3 million data entries, leverages AI for symptom prediction and mobile diagnostics. Additionally, a mindfulness-based digital intervention, MY-ENDO, was clinically validated in Denmark and is now integrated into the Lucy App, offering real-world support to patients.
«This isn’t just about tech»
Looking ahead, the FEMaLe team has outlined clear priorities: expanding clinical trials across hospitals and countries, integrating the AI system into live surgical environments, refining the user experience, and tracking long-term patient outcomes to assess real-world impact on recurrence and recovery.
Now that the project has concluded, stakeholders are exploring how to integrate these tools into national health systems, extend them beyond Europe, and potentially adapt the technologies to other complex conditions that present similar diagnostic challenges. FEMaLe’s influence is already visible in new diagnostics, such as the saliva-based Ziwig Endotest, and in projects like MIRACUM and GECCO in Germany, which are advancing the use of integrated health data and AI-driven diagnostics.
Ultimately, FEMaLe represents a new era in surgical innovation, where data, artificial intelligence, and clinical expertise converge to make the invisible visible. As Kirk puts it: «This isn’t just about tech», he concludes. «It’s about trying to end the silence and stigma around a condition that affects so many millions of women.»
References
[1] FEMaLe Consortium (2024), Finding Endometriosis using Machine Learning: Computer vision-based software for real time assessment of endometriosis, Deliverable D6.4, pp. 1-15.